This is the 9th year that May 19th will be marked as Asian American Pacific Islander (AAPI) HIV/AIDS Awareness Day, a day first established by The Banyan Tree Project (an AAPI HIV/AIDS advocacy group) and currently recognized by the US Department of Health & Human Services.
On today’s AAPI HIV/AIDS Awareness Day, here are 10 facts you may not have known about HIV/AIDS in the Asian American & Pacific Islander Community:
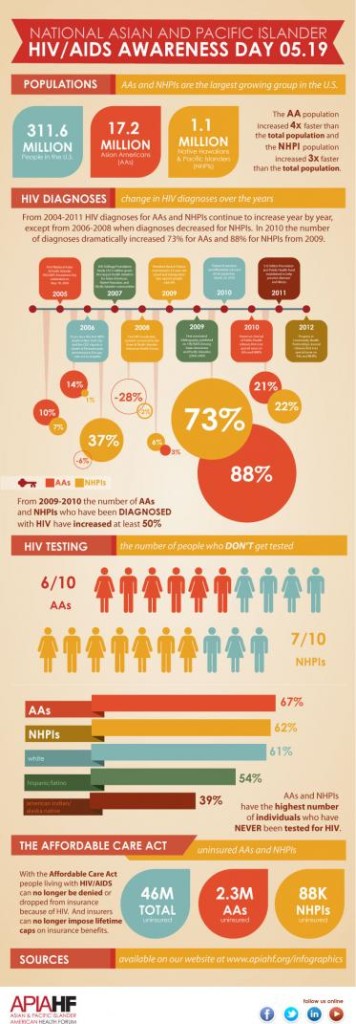
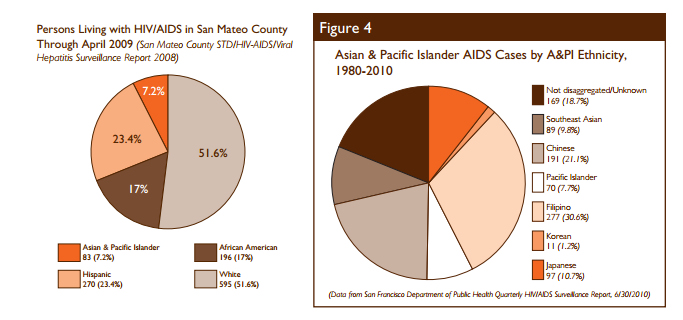
1. AAPI have among the lowest total rates of HIV / AIDS. Between 1-2% of patients living with HIV/AIDS are AAPI, however some studies suggest this number may be an underestimate due to a combination of high rates of underreporting and racial misidentification.
2. AAPI may be less likely to get tested for HIV early. The Banyan Tree Project cites a CDC report estimating that roughly 1 in 4 HIV-positive AAPIs do not know their HIV status — the highest of all race/ethnic groups — increasing transmission risks and preventing early access to important treatment.
3. Cultural stigmas against HIV discourage testing. Several studies suggest that conversation on sexual topics is stigmatized in the AAPI community, leading to low rates of sexual education and testing. In fact, only 30% of AAPI report they have ever been tested for HIV, which may in part be due to low rates of routine testing from primary care physicians as well as low availability of Asian-language HIV testing centers.
4. The Model Minority Myth may also contribute to low rates of HIV testing. AAPI are perceived as having low rates of HIV/AIDS transmission and diagnosis which is influenced in part by the Myth’s assertion that AAPI do not engage in risky sexual behaviour or are an at-risk population. Yet, as many as 90% of AAPI perceive themselves as engaging in behaviour that puts them at-risk for HIV contraction. One article reports that some healthcare providers may wrongly internalize the Model Minority Myth, and therefore choose not to advise patients to get tested if AAPI patients are in monogamous or married relationships. In fact, only 17% of AAPI women are offered an HIV test by their OB/GYN, lowest among all racial or ethnic groups.
5. AAPI are not receiving care and treatment early enough to prevent HIV from developing into AIDS. The CDC reports that 44% of HIV-positive AAPI patients develop AIDS within 1 year (highest by a few percentage points compared to other groups), suggesting that these patients aren’t getting tested soon enough. Coupled with established low and late test rates for AAPI, this high AIDS rate may be a consequence of not receiving an HIV diagnosis early enough to prevent AIDS.
6. The rate of new HIV cases is increasing for AAPI women. Whereas new cases of HIV/AIDS has remained stable or has decreased for most racial and ethnic groups, one notable exception is for AAPI women, where the rate of new HIV cases has increased by 20% in the last few years. Rates of condom use is low among AAPI women, and the failure to use adequate protection during heterosexual sex contributes to 92% of new HIV diagnoses among AAPI women.
7. Scarcity of culturally and linguistically-specific services for AAPI AIDS patients may lead to under-use. The CDC cites one study of 650 AAPI AIDS patients shows that most care being used by this population is hospital-based, while a significantly low rate take advantage of HIV case management services, housing assistance, health education or substance use treatment facilities, suggesting inadequacies in providing culturally and linguistically relevant health services for AAPIs.
8. Many AAPI sub-communities are at higher risk for HIV/AIDS. One study suggests that in San Francisco, as many as 27% of AAPI (male-to-female) trans women are living with HIV/AIDS, however this population suffers from virtually no study; more data are needed. In addition, rates of new HIV/AIDS diagnoses is higher — and routine testing rates are lower — among Native Hawaiian and Pacific Islander communities compared to averages for the general AAPI community.
9. San Francisco’s AAPI population may be experiencing a localized epidemic of HIV/AIDS, where new diagnoses exceed national averages for the AAPI population. I recently wrote about how poverty within San Francisco’s Chinese community has led to over-crowding and many health epidemics. Within San Francisco, rates of new HIV/AIDS diagnoses of AAPIs is between 5-8% of all new HIV/AIDS diagnoses, a 93% increase between 2000 – 2010 and nearly 4x the national rate.
10. You can help. Here’s what you can do:
- Get tested. Now.
- Start conversations on HIV/AIDs rates in our community by sharing this post with your friends.
- Support AAPI HIV/AIDs advocacy groups like The Banyan Tree Project (@BTPMay19), APIA Health Forum (@APIAHF), and API Wellness Center (@APIWellness).



