This past week, the CDC’s National Center for Health Statistics — a division of the CDC responsible for maintaining and publicizing national health trends for various diseases — held its annual National Conference for Health Statistics (NCHS). Members of the Asian Pacific Islander American Health Forum (APIAHF), an Asian American organization whose mission is to advocate public policy changes regarding major health concerns specifically affecting the Asian American population, was at the NCHS and tweeted several interesting facts regarding health trends in the Asian American population.
In particular, two tweets, posted back-to-back, caught my eye:
The incidence of diabetes doubled among
#AAs from 1997-2008#NHIS, the highest increase among all racial groups.@kathylimko#NCHSconference
#HeartDisease and Stroke are the leading causes of death among#AsianAmericans after#Cancer.@kathylimko#NCHSconference
The increased prevalence of diabetes and heart disease in the Asian American population is not well-known or well-publicized. In part, it may be that these diseases — rightly or wrongly — have been characterized in the popular eye as “fat people diseases”. They are seen as a complication arising from morbid obesity, which itself results from the nutritionally poor diet and low activity levels common in the Western world. Indeed for the most part science backs this up: metabolic disorders and reduced physical activity are well-recognized precursors that greatly increase risks for subsequent development of coronary artery disease, atherosclerosis and Type II diabetes.
By contrast, Asian Americans have reduced (but rising) prevalence of obesity compared to the overall U.S. population (although this is in conjunction with lower levels of physical activity as well). This perpetuates the stereotype that Asian Americans don’t suffer from health factors associated with obesity; consequently, we are virtually ignored when it comes to affecting public policy changes in this country that would address obesity and (perceived) obesity-related health problems.
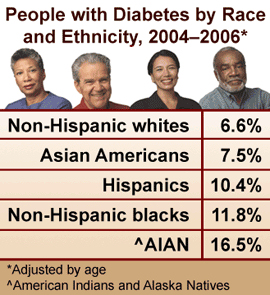
And yet, the numbers don’t lie: diabetes is more prevalent amongst Asian Americans (and other non-White minorities) compared to in the White American population. Further, the statistics presented at NCHS this year (and reported by APIAHF) indicate that diabetes (and coronary artery disease) are are a growing health concern for the Asian American population. Yet, the impact of these diseases on the Asian American population is virtually ignored by makers of public health policy, perhaps because of the general perception that Asian Americans simply don’t get diagnosed with obesity-related illnesses.
But, not only are these diseases a growing problem for Asian Americans, a new study published this week suggests that, at least when it comes to diabetes, Asian Americans may suffer a unique, more potent form of this disease that dramatically increases mortality. A study published in the Journal of the American Medical Association (JAMA) (full text, may require institutional access) collected data from over 2000 patients diagnosed with Type II diabetes and compared the mortality of these patients based on their BMI at the time of diagnosis (i.e. “normal weight” vs “overweight” patients). The authors found a surprising trend: “normal weight” patients were more likely to die during the study period than heavier patients:
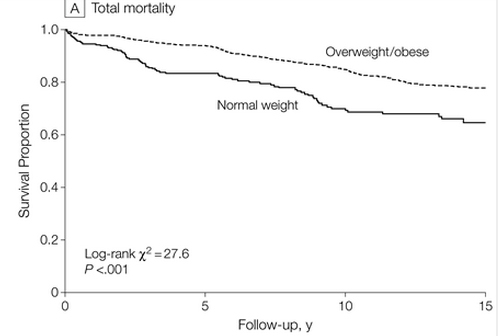
The reduced survival rate of “normal weight” Type II diabetic patients remained evident even when the authors adjusted their data to take into account smoking status, socioeconomic status, and race (White vs. Non-White; no more stratified race information was available).
Now, clearly, these data shouldn’t be used to argue that we should all attempt to become more obese. Obesity is a clear, established risk factor for diabetes, so doing this will only increase one’s likelihood of developing Type II diabetes in the first place. And, further, I don’t want to overstate the data — there’s a lot of interpretations that could be made of the author’s findings. However, these data do suggest a couple of possibilities:
1) BMI may be a terrible indicator of the health risks of obesity in Type II diabetic patients. The authors noted that a higher waist-to-hip ratio resulted in higher rates of patient death. Waist-to-hip ratio is a measure that compares a patient’s waist circumference to their hip circumference; a higher ratio means that you have higher fat deposits in your abdominal region and is a better measure of both adiposity and fat localization (which matters when it comes to how devastating that fat can be to a patient’s health). This study may indicate that it’s time for health professionals to begin the long overdue breakup with the BMI table in favour of better measures that can more accurately assess a patient’s body fat levels.
2) The data presented in the study may suggest that the BMI table is biased in its exclusion of racial information. Specifically, Asian Americans with a BMI that the BMI table would categorize as “normal weight” may actually be suffering from obesity-related health complications; in short, Asian Americans should be classified as “obese” at a lower BMI than other groups. This is the point of view suggested by some researchers at the Joslin Diabetes Center’s Asian American Diabetes Initiative.
3) The data presented in this study may suggest that Type II diabetes is a convergent disease that can arise from a combination of multiple factors. While obesity may be a driving factor for the development of disease in “overweight” patients, “normal weight” patients that nonetheless develop Type II diabetes may be developing it for different reasons. Additionally, they may be suffering from other health complications that exacerbate the progression of the disease. Either way, the form of Type II diabetes found in “normal weight” patients may actually be slightly different, and perhaps either more inherently deadly and/or less resistant to existing treatment protocols (which were largely developed through work with “overweight” diabetic patients).
And further, it’s possible that Asian American patients may be predisposed for “normal weight” diabetes due to genetic and/or lifestyle differences. CNN reports:
Overall, about 85% of people with diabetes are heavy. Gaining too much weight is a major contributor to Type 2 diabetes, since excess fat cells can affect the way the body breaks down glucose and produces insulin, but some normal weight individuals can develop the disease as well.
The elderly and people of Asian descent are more likely to be at normal weight when diagnosed, for example.
In the end, we really don’t know enough about Type II diabetes and how it affects the Asian American population. All of these data really raise more questions than answers, and ultimately demand additional attention devoted to the study of Type II diabetes in “unconventional” (i.e. non-White and/or non-obese) populations.
To date, the vast majority of clinical studies have been performed on White populations, which significantly biases our understanding of many diseases. Further, most of the statistical health data collected by scientists and the federal government fail to adequately record racial data, despite ample evidence suggesting that race and socioeconomic status both affect patient outcome in several diseases. Thus, what meager statistics we do have regarding the health status of the Asian American community suffers from low sample sizes and inadequate stratification by factors including geography, socioeconomic status, health insurance coverage, and ethnicity.
Basically, we need more and better studies of how race affects diabetes and other diseases. Even the Carnethon study that I cite in this post doesn’t specifically address how different racial backgrounds impacts the progression of Type II diabetes. We need to know how the rising rates of Type II diabetes in the Asian American population can be treated (or not) by our existing knowledge regarding Type II diabetes in other populations.
And, most importantly, we need better federal funding of science, so that those studies can be conducted.

